A Pain in the Backside
A detailed description of an ailment called haemorrhoids, their causes, symptoms and treatments.
Haemorrhoids, commonly known as piles, are a lifestyle-related condition and can have a significant impact on one’s quality of life. These are seen only in humans since we have evolved to enjoy a bipedal gait (essentially the way we walk – one foot contacting the ground after the other).
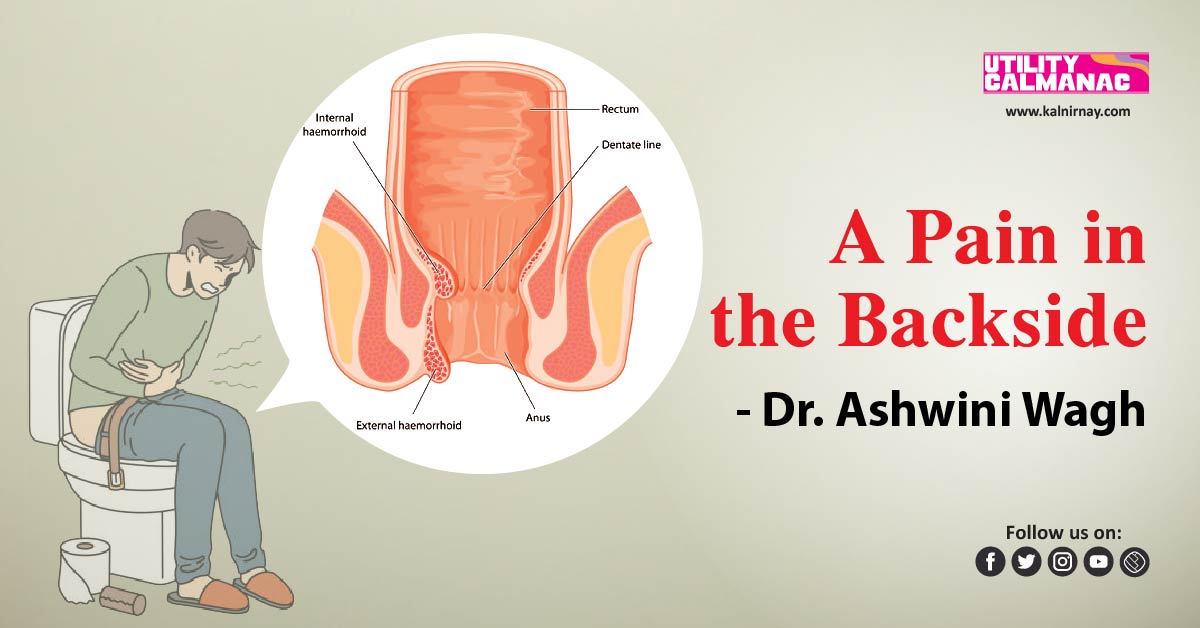
Anatomically, piles are swollen veins straining against the internal covering of the anal canal. They are universally present even in healthy individuals, but pathologic ones are those that cause symptoms in patients. When they develop inside the anal canal, they are called internal haemorrhoids, and those that develop under the skin of the anus are called external haemorrhoids.
Higher socioeconomic status is associated with an increased prevalence of haemorrhoids. Piles are aggravated by conditions that increase the intra-abdominal pressure. A fibre-deficient diet results in a prolonged gut transit time leading to harder stools, needing straining for evacuation and then the formation of piles.
Peak incidence is from 45-65 years of age. Around 50% of the population would have had haemorrhoids sometime before the age of 50 years. Almost 40% of patients with haemorrhoids do not have any complaints, hence the prevalence of haemorrhoids far outweighs the prevalence of symptoms.
Also, all anal pathologies are wrongly labelled as piles by laypersons as presentations can be quite similar. Internal haemorrhoids may cause bright red bleeding with defecation (or passing stools), which is usually painless. There is an associated sense of heaviness in the rectum. Patients usually complain of hard stools and straining while passing stools. Larger haemorrhoids cause swelling outside the anal canal. Pain is associated with infection, prolapse or strangulation of the pile mass.
Types of Haemorrhoids
- Internal haemorrhoids are lined with an internal membrane called mucosa and are painless. They are characteristically present at 3, 7 and 11 o’clock positions around the circumference of the anal canal.
Degrees of internal haemorrhoids:
- 1st degree: These haemorrhoids do not come out of the anus but have dilated blood vessels when viewed with a proctoscope.
- 2nd degree: These come out during bowel movements or straining but reduce spontaneously.
- 3rd degree: These come out during bowel movements or straining but need manual reduction.
- 4th degree: These are haemorrhoids that have come out and are irreducible even with manipulation.
- External haemorrhoids are seen outside the anus and may or may not be associated with internal haemorrhoids. They are veins lined by the skin and hence any pathology related to them can cause severe pain. Large external piles can cause pain, discomfort, swelling, irritation and itching.
Causes of Haemorrhoids
- Having a low-fibre diet
- Increased intra-abdominal pressure, causing straining while passing stools
- Chronic constipation or diarrhoea
- The regular heavy lifting of weights
- Pregnancy
Symptoms of Haemorrhoids
- Bleeding: This is bright red, painless and sometimes described as a flash in the pan.
- Swellings outside the anus: Pile masses project out. If swollen or infected, they may cause pain, difficulty in sitting and obstruction to defecation.
- Discharge and itching: Due to exposure of the internal mucosa, there may be sticky mucoid discharge, which may in turn cause itching.
- Prolapse, thrombosis or gangrene: Largely neglected piles may get infected and cause severe pain, swelling and bleeding, wounds on the pile mass and anal spasm and hence severe difficulty while passing stools.
Rectal bleeding can be an ominous symptom and should not be presumed to be always due to piles. This should prompt an immediate visit to your doctor.
A change in the consistency or colour of stools or in bowel habits and alternating diarrhoea and constipation may be symptoms of large bowel cancer and should never be ignored.
Anaemia or reduced haemoglobin due to chronic bleeding can be a result of long-standing bleeding haemorrhoids.
- Pregnancy and Haemorrhoids
Piles may form or increase during pregnancy due to the pressure of the pregnant uterus. It is important to avoid constipation during this time. In case any surgical treatment is deemed necessary, the second trimester – that is from the 4th to the 6th month – is the ideal time for the same.
Treatment
- Conservative: Dietary adjustments are the mainstay of piles management. These are long-term changes. These include adequate fluid intake, adequate fibre intake and in general avoiding foods that you know do not agree with you.
If required, some temporary laxative support may be taken. This is in tandem with using soothing creams for local application and warm baths to sit in, which help to relieve the spasm. Antibiotics and painkillers may be used only if indicated. Anaemia, which happens due to loss of blood should be treated. Some medications may cause constipation, especially iron preparations and drugs for Parkinson’s.
Respect your body. It is essential to visit the toilet as soon as you feel the urge. If neglected, the stool may harden and it will be difficult and more painful to pass later.
- Surgical: Surgical treatment can be minimally invasive or operative.
Minimally invasive treatment can be done as an in-office procedure. This includes:
- Injection sclerotherapy is where small, bleeding or remnant piles are injected with a sclerosant solution to cause fibrosis of the piles and hence shrinkage.
- Cryotherapy where extreme cold temperatures using nitrous oxide delivered by a probe is used to shrink the piles.
- Rubber band ligation of piles is done to strangulate the pile mass and cause its shrinkage.
Operative treatment requires hospitalization and anaesthesia. This includes:
- Excision and ligation of piles, which is a time-tested procedure. The larger piles are excised.
- A minimally invasive procedure for haemorrhoids involves a stapler used inside the rectum. This is suitable for larger circumferential pile masses.
- Laser haemorrhoi-dectomy, where a laser is used as a tool for shrinkage of the pile mass.
The choice of treatment depends on the patient’s condition, the severity of the piles and the comfort of the treating surgeon. A frank discussion with the treating doctor will be the best guide.
Summary
Haemorrhoids are a lifestyle-related issue. If the patient doesn’t adhere to dietary changes and requirements, the piles are likely to recur. Have adequate fibre, fluids and avoid foods that cause constipation. Post-surgery recurrence is not unknown but takes a few years and can be avoided with a healthy dietary regime.
To read more English blogs, please visit our blog section.
Dr Ashwini Wagh, M.S (Gen Surg)
The author is a consulting general surgeon.